Gestational Diabetes Diet: What to Eat & Avoid
Manage gestational diabetes with a balanced diet focusing on complex carbohydrates, lean protein, healthy fats, and portion control. Learn meal planning, blood sugar monitoring, and safe foods.
By Nooko Team

Gestational diabetes (GDM) requires careful meal planning to keep blood sugar stable. Focus on complex carbohydrates with low glycemic index (whole grains, legumes, vegetables), pair carbs with protein and healthy fats, eat small frequent meals, and limit simple sugars and refined carbs. Most people with GDM can manage blood sugar through diet alone, though some need insulin. Work with a registered dietitian for a personalized meal plan.1
Understanding Gestational Diabetes
Gestational diabetes develops during pregnancy when your body can’t produce enough insulin to handle increased blood sugar from pregnancy hormones. It affects about 6-9% of pregnancies and typically resolves after delivery, though it increases risk of type 2 diabetes later in life.2
Goals:
- Keep fasting blood sugar under 95 mg/dL
- Keep 1-hour post-meal blood sugar under 140 mg/dL
- Keep 2-hour post-meal blood sugar under 120 mg/dL
Key Principles of GDM Diet
1. Choose Complex Carbohydrates
What they are: Carbs with fiber that break down slowly, preventing blood sugar spikes.
Best choices:
- Whole grains: Brown rice, quinoa, oats, barley, whole wheat bread
- Legumes: Lentils, chickpeas, black beans, kidney beans
- Starchy vegetables: Sweet potatoes, corn, peas (in moderation)
- Non-starchy vegetables: Broccoli, spinach, peppers, tomatoes, zucchini (unlimited)
Limit or avoid:
- White bread, white rice, white pasta
- Sugary cereals
- Pastries, cookies, cakes
- Candy and sweets
- Regular soda and fruit juice3
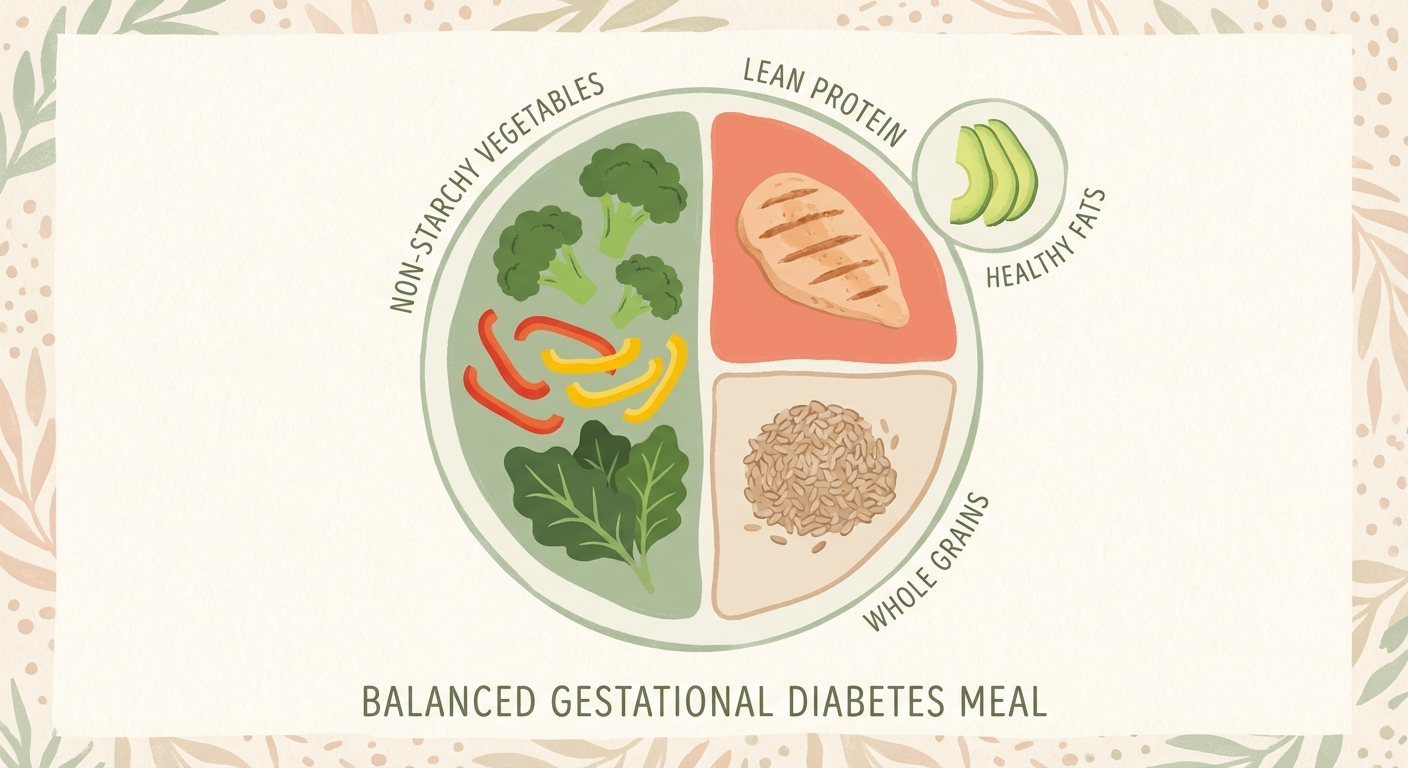
2. Pair Carbs with Protein and Fat
Why: Protein and healthy fats slow carb absorption, preventing blood sugar spikes.
Examples:
- Apple with peanut butter
- Whole grain crackers with cheese
- Oatmeal with nuts and Greek yogurt
- Brown rice with chicken and avocado
Good protein sources:
- Lean meats: Chicken, turkey, lean beef
- Fish: Salmon, cod, tilapia (follow pregnancy fish guidelines)
- Eggs
- Greek yogurt
- Legumes and beans
- Tofu and tempeh
- Nuts and nut butters
Healthy fats:
- Avocado
- Nuts and seeds
- Olive oil
- Fatty fish (salmon, sardines)
- Nut butters4
3. Control Portions
Why: Even healthy carbs raise blood sugar if portions are too large.
Guidelines:
- 1/2 to 1 cup complex carbs per meal
- Fill half your plate with non-starchy vegetables
- 1/4 plate protein
- 1/4 plate complex carbs
Use your hand as a guide:
- Protein: Palm-sized portion
- Carbs: Cupped handful
- Fats: Thumb-sized portion
4. Eat Small, Frequent Meals
Why: Prevents blood sugar from getting too high or too low.
Schedule:
- Breakfast
- Mid-morning snack
- Lunch
- Afternoon snack
- Dinner
- Evening snack (especially important)
Evening snack: Include protein and complex carb (like whole grain crackers with cheese) to prevent overnight blood sugar drop and morning spike.
5. Limit Sugary Foods
Avoid or severely limit:
- Regular soda
- Fruit juice (even 100% juice)
- Sweetened beverages
- Candy
- Cookies, cakes, pastries
- Ice cream
- Sweetened yogurt
- Dried fruit (concentrated sugar)
Better choices:
- Water, sparkling water
- Unsweetened tea
- Whole fruits in small portions
- Plain Greek yogurt with berries
Sample GDM Meal Plan
Breakfast
Option 1:
- 2 scrambled eggs
- 1 slice whole wheat toast
- 1/2 avocado
- Small handful of berries
Option 2:
- Greek yogurt (plain, not flavored)
- 1/4 cup low-sugar granola
- Handful of berries
- Sprinkle of nuts
Mid-Morning Snack
- Apple slices with 1 tablespoon peanut butter
- OR: Cheese stick with 5-6 whole grain crackers
Lunch
- Large salad with mixed greens
- Grilled chicken breast
- Chickpeas
- Olive oil and vinegar dressing
- 1/2 cup quinoa
Afternoon Snack
- Carrot and cucumber sticks
- 1/4 cup hummus
Dinner
- Baked salmon (4 oz)
- Roasted broccoli and cauliflower
- 1/2 cup brown rice
- Small side salad
Evening Snack
- Whole grain crackers (6-8)
- String cheese
- OR: Small apple with almond butter
Foods to Emphasize
Non-starchy vegetables (unlimited):
- Leafy greens, broccoli, cauliflower, peppers, tomatoes, cucumbers, zucchini, asparagus, green beans
Lean proteins:
- Chicken, turkey, fish, eggs, Greek yogurt, cottage cheese, tofu
Healthy fats:
- Avocado, nuts, seeds, olive oil, fatty fish
Complex carbs (measured portions):
- Whole grains, legumes, sweet potato (with skin)
Berries (lower sugar fruit):
- Strawberries, blueberries, raspberries, blackberries
Blood Sugar Monitoring
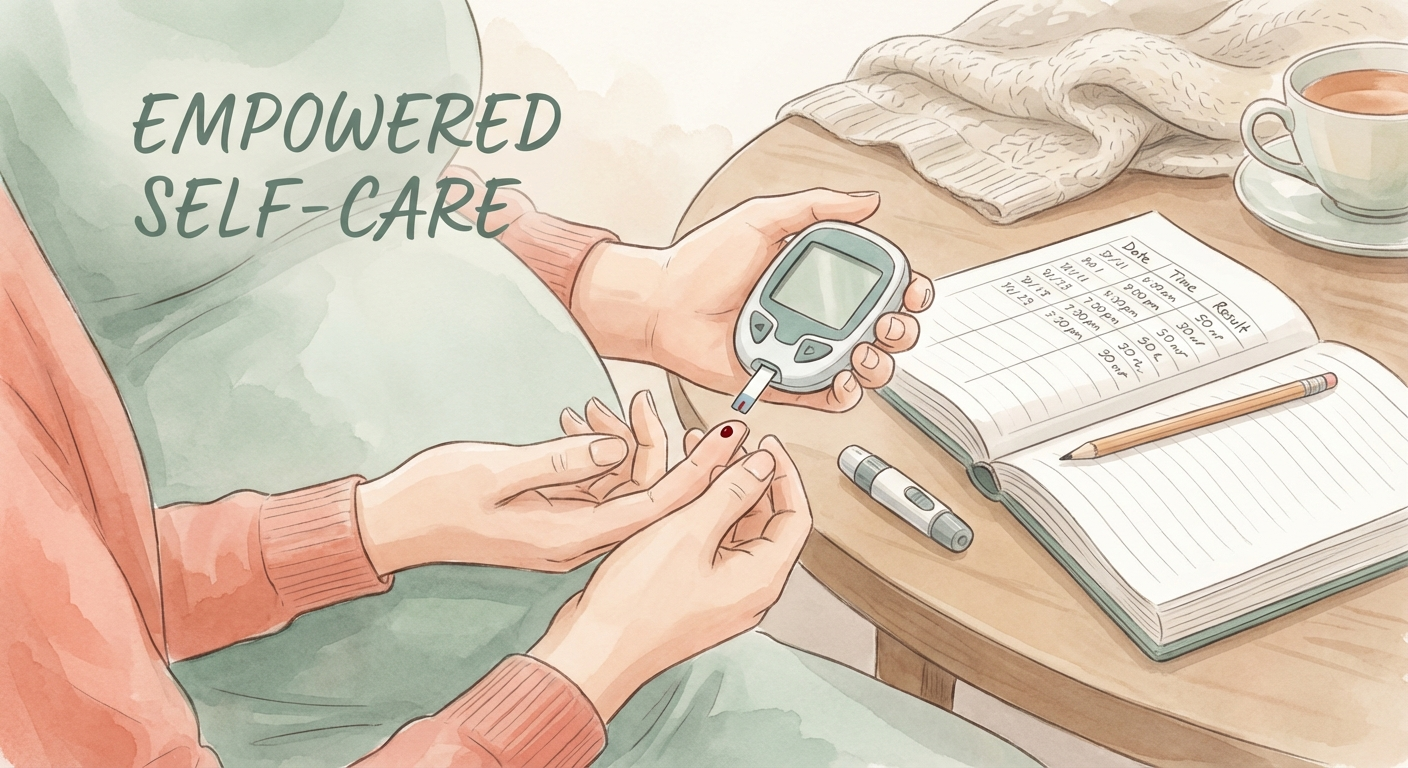
Testing schedule (typical):
- Fasting: Upon waking
- 1-hour or 2-hour post-meal: After breakfast, lunch, dinner
Keep a log: Record what you ate, portion sizes, and blood sugar readings to identify patterns.5
Share with your healthcare team: Regular monitoring helps adjust your plan.
When Diet Alone Isn’t Enough
About 10-20% of people with GDM need insulin or medication in addition to diet.6 This doesn’t mean you failed—some bodies simply can’t produce enough insulin during pregnancy regardless of diet.
Signs you may need medication:
- Consistently high blood sugar despite following meal plan
- Unable to keep fasting blood sugar under 95 mg/dL
- Unable to keep post-meal readings in target range
Exercise and GDM
Moderate exercise (walking, swimming, prenatal yoga) helps lower blood sugar. Aim for 30 minutes most days of the week, with your provider’s approval.7
Track Your GDM Management with Nooko
Nooko helps you log meals, track blood sugar readings, identify patterns, and share data with your healthcare team. Monitor your carb intake, record blood glucose levels, and get personalized meal suggestions that keep blood sugar stable while ensuring proper nutrition for you and your baby.
Download Nooko on the App Store | Get Nooko on Google Play
References
Footnotes
-
American College of Obstetricians and Gynecologists. (2025). “Gestational Diabetes.” https://www.acog.org/womens-health/faqs/gestational-diabetes ↩
-
CDC. (2024). “Gestational Diabetes.” https://www.cdc.gov/diabetes/gestational-diabetes/index.html ↩
-
American Diabetes Association. (2024). “Eating Well with Gestational Diabetes.” https://diabetes.org/food-nutrition/eating-well-gestational-diabetes ↩
-
Academy of Nutrition and Dietetics. (2024). “Gestational Diabetes Nutrition Therapy.” Journal of the Academy of Nutrition and Dietetics. ↩
-
ACOG. (2025). “Gestational Diabetes.” ↩
-
ACOG. (2025). “Gestational Diabetes.” ↩
-
American College of Obstetricians and Gynecologists. (2024). “Exercise During Pregnancy.” https://www.acog.org/womens-health/faqs/exercise-during-pregnancy ↩
Ready to track your pregnancy?
Join expecting parents using Nooko to track every milestone together.
Join the Nooko Beta →Get Weekly Pregnancy Tips
Expert advice for every stage of your journey
No spam. Privacy policy. Unsubscribe anytime.